Sling surgery for stress urinary incontinence is best deferred until a woman has completed her family as further pregnancies and childbirth can reverse the effects of surgery and result in recurrent stress incontinence.
What is a Pubovaginal Sling to treat Stress Urinary Incontinence?
A pubovaginal sling is thin ribbon of tissue that lies under the neck of the bladder (at the junction of the bladder and the urethra which is the tube draining urine from the bladder). The sling acts by providing support under the bladder neck when there is a rise in intraabdominal pressure (e.g. with cough, exercise, lifting) to help prevent stress incontinence.
The pubovaginal sling is also known as a fascial or natural tissue sling because it is made of tissue rather than mesh material like the synthetic mid-urethral slings. The most common source of the pubovaginal sling material is a woman’s own tissue as the sling is usually harvested from the rectus fascia (a dense fibrous material overlying the abdominal muscles) through an incision in the lower abdomen. The sling measures around 8 cm and is placed under the bladder neck by a separate incision made in the vagina. Sutures are used to tie the ends of the sling over the abdominal muscles.
Surgery for a pubovaginal sling is not minimally invasive (like synthetic mid-urethral sling surgery) as the sling needs to be harvested and is obtained through an abdominal incision which results in a longer stay in hospital and longer recovery time than mid-urethral sling surgery.
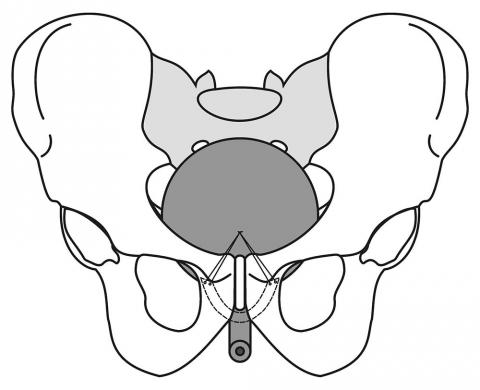
Diagram of a Pubovaginal or Fascial sling to treat stress urinary incontinence.
Copyright Dr Karen McKertich - Not for use without attribution.
What does the procedure involve?
Pubovaginal fascial sling surgery is performed in hospital under a general anaesthetic. The procedure is combined with a cystoscopy to confirm correct sling placement.
Women are usually admitted to hospital for around 4-5 days due to the abdominal wound and dissection. A catheter (urinary drainage tube) as well as a vaginal pack (wound dressing) is left for up to a couple of days after surgery.
If the patient passes urine well after removal of the catheter (urinary drainage tube) after the procedure, they can go home.
Restriction in activity is required for at least 4 to 6 weeks after surgery to allow the sling to scar into position and maximise the success of surgery.
How successful is a Pubovaginal Sling in treating Stress Urinary Incontinence in Women?
Pubovaginal fascial slings cure or significantly improve stress urinary incontinence in about 85 to 90% of women. Studies have shown that the results are durable in the vast majority of patients.
What are the potential side effects of a Pubovaginal Sling surgery for Stress Incontinence?
All surgery for stress urinary incontinence has potential side effects.
Specific risks associated with pubovaginal sling surgery include:
- Failure to improve or rarely worsening of stress urinary incontinence
- Development of new overactive bladder (OAB) symptoms or worsening of pre-existing OAB symptoms
- Damage to nearby structures on insertion of the sling such as the bladder, urethra, blood vessels or bowel
- Difficulty in urination that may result in a need to loosen or divide the sling or the need for temporary intermittent self-catheterisation to drain the bladder
- Urinary tract infection
- Wound infection
- Abdominal discomfort related to the sling
- Discomfort related to sexual intercourse
Are there other alternatives to treat Stress Urinary Incontinence in Women?
Many treatment options exist for women with stress urinary incontinence including:
- Pelvic floor physiotherapy
- Weight loss if overweight
- Continence devices used vaginally
- Sling surgery with synthetic mid-urethral slings
- Injectable agents
- Colposuspension





